In a world increasingly driven by technology, healthcare is undergoing a remarkable transformation. Smart pills and wearable biosensors are two pioneering innovations that are poised to redefine patient monitoring. These advanced tools allow for real-time data collection, non-invasive health tracking, and proactive medical interventions. From managing chronic diseases to enhancing diagnostic accuracy, smart pills and biosensors could mark the beginning of a more personalized, predictive, and preventive healthcare system.
This blog explores the science behind these technologies, their current applications, and what the future may hold for medicine as we integrate smart health monitoring into everyday life.
Understanding Smart Pills
What Are Smart Pills?
Smart pills, also known as ingestible sensors or digital pills, are miniature electronic devices embedded within a capsule. Once swallowed, they travel through the gastrointestinal (GI) tract and collect vital health data. Some smart pills are designed to monitor medication adherence, while others gather physiological data such as pH levels, temperature, and pressure.
How Do They Work?
Smart pills generally consist of:
- A biosensor
- A microprocessor
- A transmitter
- A power source (often using stomach fluids)
The ingested pill transmits data to a wearable patch or smartphone app, allowing physicians and patients to track health metrics in real-time. The pill disintegrates or passes naturally after completing its function.
Key Players and Products
- Proteus Digital Health (now closed): Developed one of the first FDA-approved smart pills.
- CapsoCam Plus: A capsule endoscopy system for GI tract imaging.
- PillCam (Medtronic): Enables visualization of the small intestine for diagnostics.
Exploring Wearable Biosensors
What Are Wearable Biosensors?
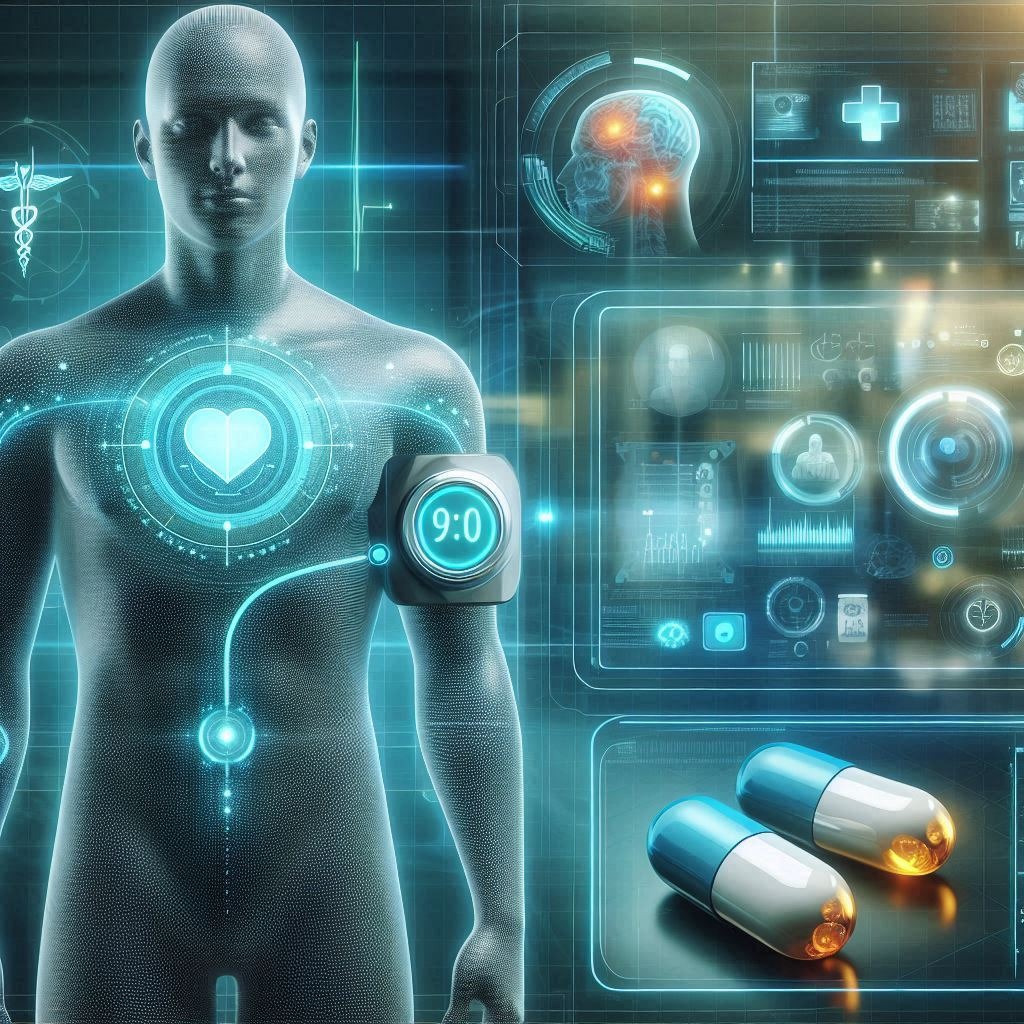
Wearable biosensors are compact, portable devices that monitor and transmit health-related data. These gadgets are typically worn on the wrist, arm, chest, or embedded in clothing. They can measure a wide range of biological indicators, including heart rate, blood glucose levels, oxygen saturation, and even sweat composition.
Types of Wearable Biosensors
- Electrochemical Sensors: Detect chemical compounds in sweat, saliva, or interstitial fluid.
- Optical Sensors: Use light to measure metrics like oxygen saturation and pulse rate.
- Motion Sensors: Track activity, posture, and movement.
- Temperature Sensors: Monitor body temperature to detect fever or metabolic fluctuations.
Real-World Applications
- Diabetes Management: Continuous glucose monitors (CGMs) like Dexcom and FreeStyle Libre.
- Cardiovascular Monitoring: Wearables like Apple Watch and Fitbit detect arrhythmias.
- Mental Health: Biosensors track stress levels via heart rate variability.
- Fitness and Lifestyle: Track steps, sleep patterns, calories burned.
Integration in Clinical Practice
Remote Patient Monitoring (RPM)
RPM is becoming a standard practice for managing patients with chronic illnesses. Smart pills and biosensors provide continuous health updates, reducing the need for frequent hospital visits.
Hospital-at-Home Models
With accurate monitoring tools, healthcare providers can manage patients at home post-surgery or during long-term treatments, decreasing hospital load and costs.
Clinical Trials and Research
Wearables and ingestibles offer real-time health data, improving the precision and reliability of clinical trials. This data-centric approach accelerates drug development and approval processes.
Benefits and Challenges
Benefits
- Early Detection: Identify potential health issues before they become critical.
- Personalized Treatment: Data enables tailored healthcare plans.
- Improved Compliance: Smart pills remind patients to take medication.
- Cost Reduction: Decreases hospital visits and emergency care.
Challenges
- Privacy Concerns: Handling of sensitive health data.
- Technical Limitations: Battery life, data accuracy, and connectivity.
- Regulatory Hurdles: FDA approvals and safety validations.
- User Adoption: Elderly and less tech-savvy individuals may face difficulties.
The Future of Patient Monitoring
Integration with AI and Big Data
Combining biosensor data with AI algorithms enables predictive analytics. For example, AI can detect patterns indicating early signs of heart failure or infection.
Interoperability and Healthcare Ecosystems
Unified platforms that integrate smart pill and biosensor data with electronic health records (EHRs) will streamline patient care and improve communication among healthcare providers.
Next-Gen Innovations
- Implantable Biosensors: Permanent sensors for chronic disease management.
- Nanotechnology Integration: More sensitive and specific sensors.
- Smart Tattoos: Temporary electronic tattoos that provide biosensing functions.
Ethical and Societal Considerations
Informed Consent and Data Ownership
Patients must understand how their data is collected, used, and stored. Legal frameworks must evolve to safeguard individual rights.
Equity and Accessibility
Tech-driven healthcare must avoid widening the gap between populations with varying access to digital tools. Policies should focus on inclusive access.
Human-AI Collaboration
As AI interprets patient data, a balance must be struck between machine efficiency and human empathy in care delivery.
Conclusion: A Paradigm Shift in Healthcare
Smart pills and wearable biosensors are not just technological novelties—they are fundamental building blocks for the future of personalized, connected, and proactive healthcare. While challenges remain, the benefits are vast: early diagnosis, better disease management, and reduced healthcare costs. As these tools evolve and integrate with broader health ecosystems, they hold the potential to make healthcare more human-centered, despite being driven by machines.
The future is already here, and it’s being swallowed and worn.






+ There are no comments
Add yours