The global burden of cancer is escalating at an unprecedented rate, and timely, accurate diagnosis has never been more crucial. In recent years, Artificial Intelligence (AI) has emerged as a transformative force in the field of oncology. From automating image analysis to predicting tumor behavior, AI-driven tools are increasingly integrated into cancer diagnostics. However, with this innovation comes a host of ethical, practical, and regulatory questions that demand attention.
This blog explores the dual-edged role of AI in cancer diagnosis, offering insights into its potential, limitations, and the ethical dilemmas it introduces. As an experienced blog writer with a decade of expertise, my aim is to present these findings in a balanced, clear, and engaging manner.
The Growing Role of AI in Cancer Diagnosis
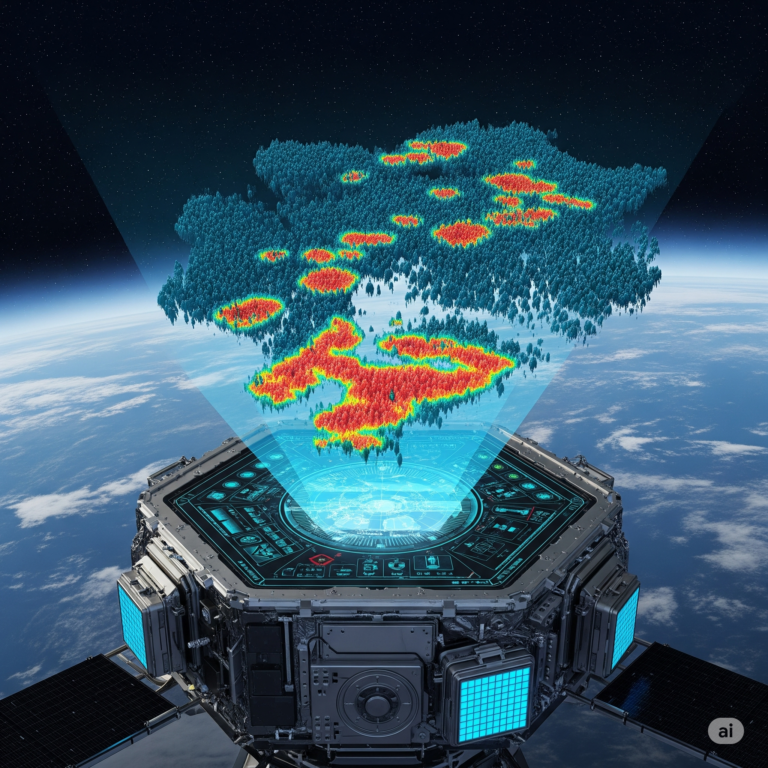
Pattern Recognition and Radiology
One of AI’s most promising applications in oncology lies in radiology. Algorithms trained on thousands of medical images can detect anomalies in mammograms, CT scans, and MRIs with near-human accuracy. Deep learning models, particularly convolutional neural networks (CNNs), excel at identifying subtle patterns that may escape even experienced radiologists.
Histopathology and Digital Slides
AI has revolutionized histopathological analysis by digitizing biopsy slides. Tools like PathAI and Google’s LYNA assist pathologists by highlighting suspicious regions, reducing human error, and speeding up the diagnosis process.
Genomics and Predictive Modeling
AI algorithms can also analyze genomic data to identify mutations associated with specific cancers. By integrating genetic, clinical, and imaging data, AI models can predict disease progression and suggest personalized treatment options.
Ethical Considerations in AI-Powered Diagnosis
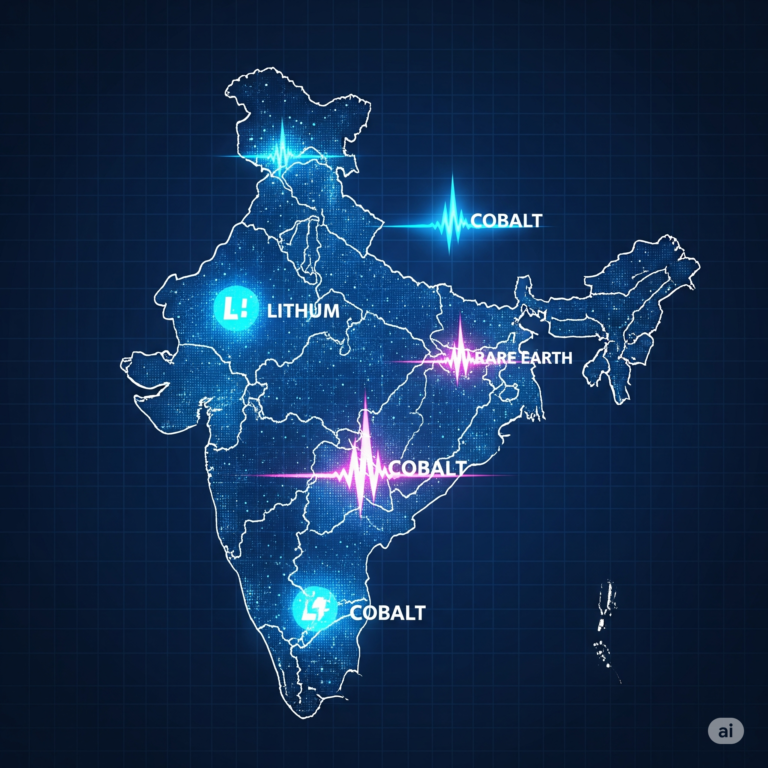
Bias in Training Data
AI systems are only as good as the data they are trained on. If training data lacks diversity—such as underrepresentation of certain ethnic groups—diagnostic accuracy may be compromised. This raises serious concerns about healthcare equity.
Transparency and Explainability
Many AI models operate as “black boxes,” providing results without a clear explanation of how they arrived at their conclusions. This lack of transparency can undermine trust between doctors and patients.
Accountability and Liability
Who is responsible if an AI model makes an incorrect diagnosis? Is it the developer, the hospital, or the physician who relied on the tool? These questions highlight the need for clear legal frameworks.
Informed Consent and Data Privacy
Patients must be informed when their data is used to train AI models. Additionally, stringent safeguards must be in place to protect sensitive health information from breaches.
Practical Challenges in Implementation
Integration into Clinical Workflows
For AI tools to be effective, they must seamlessly integrate into existing healthcare systems. This includes compatibility with Electronic Health Records (EHRs) and interoperability across various departments.
Cost and Accessibility
Developing and maintaining AI systems is expensive. There is a risk that only well-funded institutions will benefit from this technology, widening the gap between different healthcare providers.
Continuous Learning and Validation
AI models must be continuously updated and validated to maintain accuracy, especially as new medical data and imaging techniques emerge.
The Road to Ethical AI in Oncology
Regulatory Guidelines
Organizations like the FDA and EMA are working to create guidelines for the ethical use of AI in medicine. These regulations aim to ensure safety, effectiveness, and transparency.
Collaborative Human-AI Models
The future likely lies in hybrid models where AI assists rather than replaces human judgment. This ensures that ethical reasoning, empathy, and clinical experience remain integral to patient care.
Training and Education
Healthcare professionals must be educated about how AI systems work. Understanding the strengths and limitations of AI tools is essential for their responsible use.
Case Studies and Real-World Applications
IBM Watson for Oncology
IBM Watson was designed to analyze patient data and suggest treatment options. While it faced criticism for inaccuracies, it sparked crucial conversations about AI’s role in oncology.
DeepMind and Moorfields Eye Hospital
DeepMind developed an AI system capable of diagnosing over 50 eye conditions. Though not cancer-related, it demonstrated the potential of AI in medical diagnostics.
Google’s Breast Cancer AI Model
A 2020 study published in Nature showcased Google Health’s AI model that outperformed radiologists in breast cancer detection. It reduced both false positives and false negatives.
Future Outlook: A Balanced Approach
Emphasis on Ethical Design
Ethical considerations must be integrated from the design phase itself. This includes using diverse datasets, creating transparent models, and involving ethicists in development teams.
Public Engagement and Policy Making
Public discourse and policy-making should go hand in hand. Patients, clinicians, ethicists, and policymakers must collaboratively shape the future of AI in healthcare.
Global Collaboration
AI’s potential in oncology is a global concern. Cross-border collaborations can help create standardized protocols and share best practices.
Conclusion
AI-driven cancer diagnosis holds transformative potential. It can speed up detection, improve accuracy, and personalize treatment—three pillars of effective cancer care. However, the path forward must be navigated carefully, ensuring that ethical principles, patient trust, and equitable access are never compromised.
As we stand on the brink of this technological revolution, a balanced approach—one that combines innovation with introspection—will be the key to unlocking the true promise of AI in oncology.
Key Takeaways
- AI is increasingly used in cancer diagnostics, from imaging to genomics.
- Ethical concerns include bias, transparency, accountability, and data privacy.
- Practical hurdles involve cost, integration, and continuous learning.
- Regulatory guidelines and human-AI collaboration are vital for ethical deployment.
- A balanced, inclusive approach is essential to harness AI’s full potential in oncology.








+ There are no comments
Add yours